.jpeg)
Inside the eye, just behind the coloured iris, is the intra ocular lens. Ideally the lens should be crystal clear and helps focus light accurately onto the retina (Fig 1). As the lens ages it often becomes less transparent (Fig 2). A cataract is simply this intra ocular lens becoming cloudy.

Numerous types of cataracts exist, some affecting vision more than others.
The most common age-related cataract is the ‘Nuclear Sclerotic’ where the entire lens become yellow. This gives everything a browny haze and can produce large changes in spectacle powers.
See below from left to right:
1. Nuclear Sclerotic 2. Posterior Subcapsular 3. Cotical
There are no hard and fast rules on when to remove cataracts. Cataract surgery is far less risky than previously, allowing them to be removed at an earlier stage, well before vision is badly affected. We will advise you, but your ‘Quality of Life’ and opinions must drive referral decisions. If you are content with your quality of vision, and your visual needs are met, cataract extraction should not be considered. However, if the cataract is causing you to struggle with important aspects of life such as night driving or reading then removal could be recommended, irrespective of how well you see on a ‘high contrast’ vision chart.
Age related cataracts can evolve slowly. Patients become frustrated with their spectacles which underperform. People often feel the need to clean or adjust their glasses in an attempt to improve vision quality; while being unable to pinpoint the exact cause.
There may be quite rapid changes in spectacle power as the cataract makes the intraocular lens power change. More frequent monitoring may be recommended.
Cataracts can induce ‘disability’ glare. Bright sources of light directly in front of you such as headlights and reflections off wet road surfaces can be distressing.
Vision Cataracts can impact ‘Low Contrast’ (poor light conditions) vision more profoundly. Night driving, foggy and winter conditions can be very difficult.
Cataracts, because they act like fi lters, also make you very light dependent. A good stand-light, behind you (i.e., not glare), can greatly improve reading performance.
Previously the role of the optician, pre and post cataract extraction, was simply to check your vision and report findings to ophthalmology. This is unacceptable. Unacceptable when monitoring cataract progression. Unacceptable when referring for extraction. Absolutely unacceptable at post-surgical outcome review.
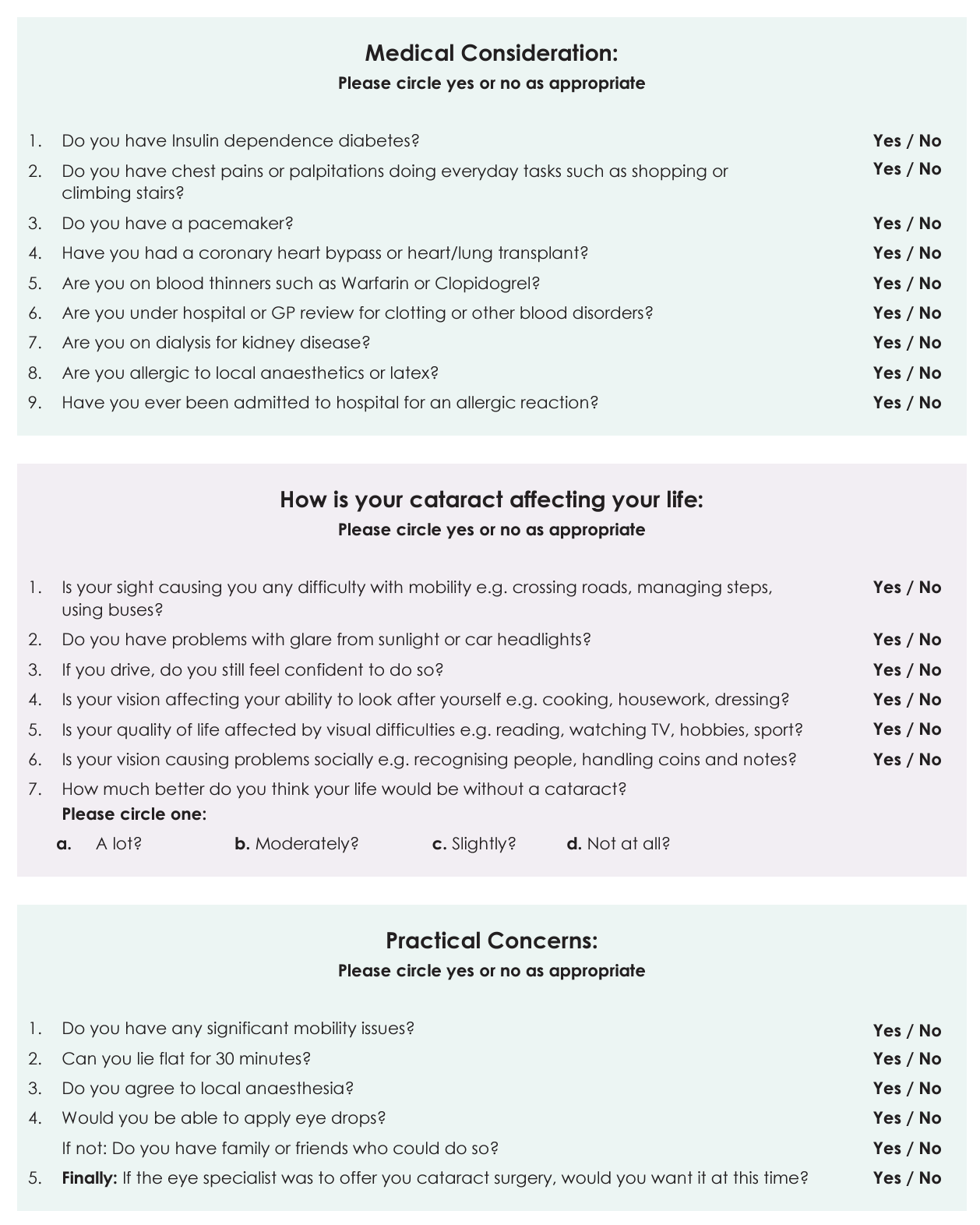
Prior to Referral: Surgeons will better serve you if they have a complete picture of you and your eye health prior to physical examination. Seemingly simple things, such as ensuring referral reflects your personal quality of life difficulties, are essential and take time. Page 4 includes lifestyle questionnaires and health considerations for cataract referral refinement.
The Medical Optometrist must ensure all medications are considered and possible risks identified. Clinically we must search for, and eliminate, alternate problems possibly contributing to your poorer vision.
Further it is important to identify risk factors for surgery; coincidental ocular conditions, potentially complicating or even preventing surgery, or affecting visual outcomes.
1. In-depth medical level assessment of general health and medications.
2. ‘Quality of Life’ questionnaires are helpful, and responses included in referrals.
3. Assessment of ‘Low Contrast’ vision, rather than black/white high contrast vision is more indicative of ‘real life’ visual problems.
4. Assessment of lid health. Lids can be a source of infection during surgery and managing the risk is important.
5. Certain corneal (clear window) conditions make cataract extraction more challenging, and surgeons should be pre-informed.
6. As cataracts develop and swell, they can restrict outflow of intra-ocular fluid. Specialist scans of the drainage angles can highlight potential problems before referral.
7. Scans are also recommended to ensure the retina itself is healthy. Very subtle problems, not necessarily visible through the cataract, may not stop cataract extraction, but may change visual outcome expectations.
Post cataract surgery community follow-up: In the past the role of the optician, at post cataract review, was simply to check your vision and report the fi ndings to ophthalmology. This was, arguably, acceptable as the patient would be examined by the surgeon personally within days.
This has not been the case for many years now; all reviews are remote. This liberates time for the hospital and is also far more convenient for the patient. This strategy, however, carries the risk surgical mishap could go undetected; only the case if optometrists do not enhance their roles and clinical techniques.
Consequently, we insist on a ‘Medical’, rather than simple optical, grade assessment. We will thoroughly assess your ocular health and surgical outcomes, reporting adverse reactions immediately to ophthalmology. As ‘Medical’ optometrists we may also commence treatment for some post-surgical complications immediately, speeding up resolution.
Below are two examples of post extraction complications identifi ed and managed by ‘Medical’ Optometrists at Aarons. The surgeons were informed but treatment commenced immediately.

As vital as this post-surgical investigation is, the RVI does not pay for the heightened responsibilities and advanced investigative techniques taken on by some Optometrists.
(Downloadable PDF at top of page)